Determinants of Health
Determinants of Health: Understanding the Forces That Shape Our Well-being
Determinants of Health is more than the absence of disease—it is a complex interplay of physical, mental, social, and environmental factors. Why do some people live longer, healthier lives while others face chronic illnesses and early mortality, despite access to the same healthcare system?
The answer lies not only in genetics or medical care, but in what public health professionals call the determinants of health—the broad range of personal, social, economic, and environmental factors that influence health outcomes.
In this in-depth article, we explore the multifaceted concept of health determinants, examine their categories, highlight real-world examples, and discuss how understanding these determinants is key to building healthier individuals, communities, and nations.
What Are Determinants of Health?
Determinants of health are the wide array of factors that affect an individual’s or population’s health. These go beyond the traditional view of health as a purely biological phenomenon and consider the context of people’s lives—where they are born, grow, live, work, and age.
The World Health Organization (WHO) defines them as “the range of personal, social, economic, and environmental factors that determine the health status of individuals or populations.”
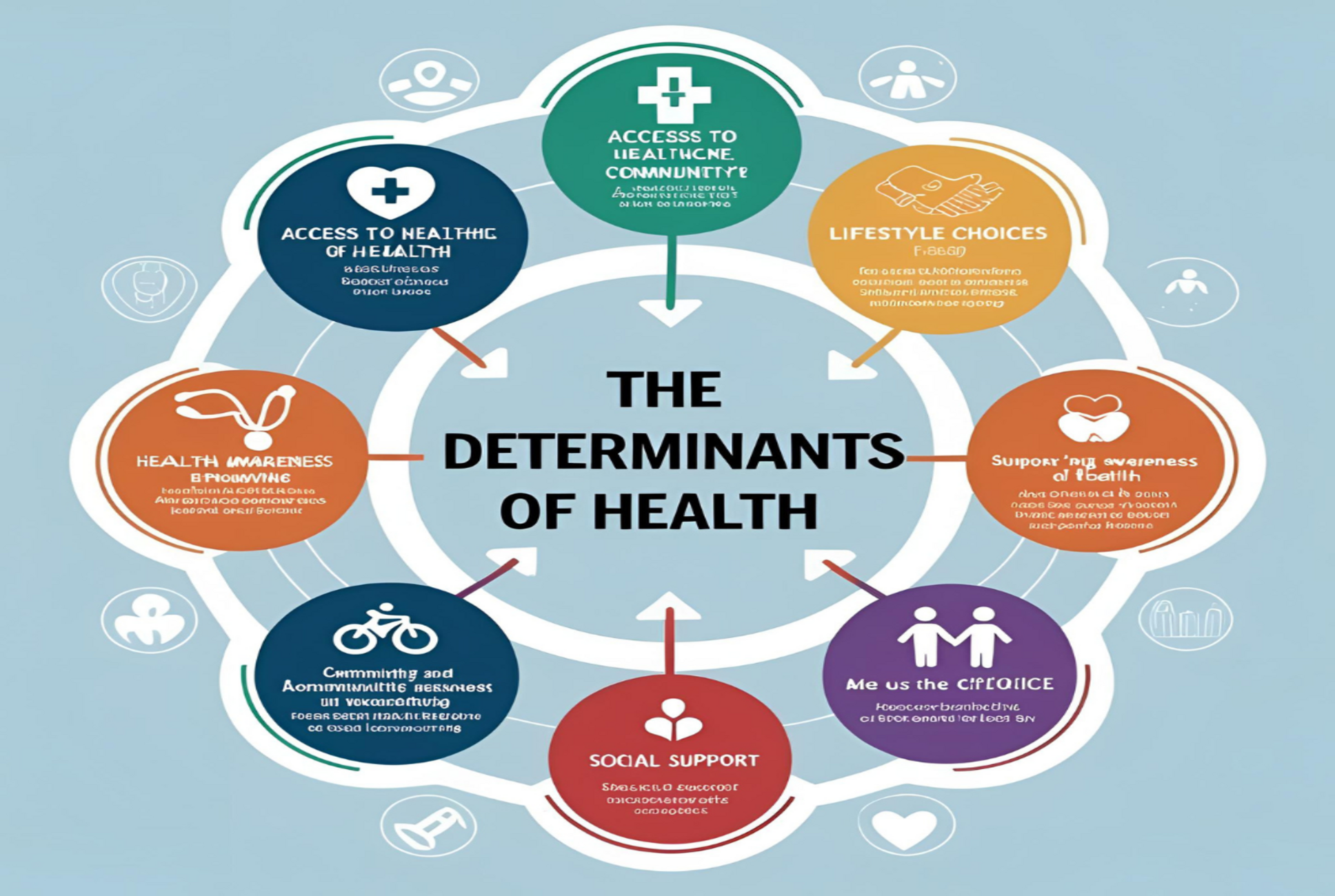
The Five Major Categories of Health Determinants
Public health experts often group determinants of health into five broad, interconnected categories:
- Social and Economic Environment
- Physical Environment
- Health Behaviors
- Access to Health Services
- Genetics and Biology
Each of these determinants plays a critical role in shaping health outcomes. Let’s explore them in detail.
1. Social and Economic Environment
Perhaps the most powerful predictor of health is socioeconomic status (SES)—a measure that includes income, education, and occupation. A person’s social and economic position deeply influences nearly every other aspect of health.
Income and Poverty
People living in poverty are more likely to experience:
- Poor nutrition
- Substandard housing
- Limited access to healthcare
- Greater exposure to violence
- Increased stress
These factors compound over time, leading to worse health outcomes.
Education
Education equips individuals with knowledge, critical thinking, and problem-solving skills. Educated individuals are more likely to:
- Engage in healthy behaviors
- Seek preventive care
- Have better employment and income
- Understand medical instructions
Employment and Job Security
Jobs that provide fair wages, safety, health benefits, and work-life balance support good health. Conversely, unemployment or job insecurity can cause stress, anxiety, and reduced access to care.
Social Support and Community Networks
Strong social ties are protective. People with supportive families and communities enjoy better mental health, reduced loneliness, and stronger immune systems.
2. Physical Environment
The surroundings where people live, work, and play can significantly impact their health.
Air and Water Quality
Exposure to pollutants increases the risk of respiratory diseases, cardiovascular problems, and certain cancers. Clean air and safe drinking water are basic human rights and critical for public health.
Housing
Poor housing conditions—such as mold, dampness, overcrowding, or exposure to toxins like lead—can lead to respiratory issues, mental health disorders, and communicable diseases.
Neighborhood Safety and Infrastructure
Safe neighborhoods with walkable streets, access to parks, and low crime rates promote physical activity and mental well-being. Conversely, high-crime areas foster chronic stress and limit mobility.
Access to Healthy Food
Areas known as food deserts, where fresh produce and nutritious food are scarce or expensive, increase the likelihood of obesity and diet-related diseases.
3. Health Behaviors
Individual lifestyle choices are major determinants of health, though often influenced by other factors like environment, culture, and education.
Tobacco Use
Smoking is linked to heart disease, cancer, and lung conditions. Public health campaigns have successfully reduced smoking rates, but disparities remain.
Alcohol and Substance Use
Excessive alcohol consumption and drug use lead to liver disease, injuries, mental illness, and social problems. Community-based prevention programs are essential.
Physical Activity
Regular exercise reduces the risk of many chronic conditions, including heart disease, diabetes, and depression. But safe spaces and time to exercise are not equally available to all.
Diet and Nutrition
A healthy diet rich in fruits, vegetables, and whole grains supports longevity. However, food affordability, advertising, and cultural norms influence dietary choices.
Sexual Behavior
Safe sexual practices help prevent sexually transmitted infections (STIs) and unintended pregnancies. Education and access to reproductive health services are vital.
4. Access to Health Services
While not the only determinant of health, access to healthcare remains a cornerstone of disease prevention, treatment, and management.
Availability
Are healthcare services physically present in the community? Rural or underserved areas often lack hospitals or specialist care.
Affordability
Cost remains a major barrier. Even in countries with universal health coverage, out-of-pocket expenses can deter people from seeking care.
Acceptability
Cultural sensitivity and patient-centered care ensure that services meet the needs of diverse populations.
Accessibility
Can people easily reach services? Transportation, language barriers, and health literacy all play roles in accessibility.
When healthcare is inaccessible, treatable conditions can escalate into serious problems, increasing long-term costs and suffering.
5. Genetics and Biology
Our genetic makeup influences susceptibility to certain diseases, longevity, and how we respond to treatment.
Inherited Conditions
Genetic disorders like cystic fibrosis, sickle cell anemia, and Huntington’s disease are passed from one generation to another.
Biological Factors
Age, sex, and immune function affect health risks. For example:
- Older adults face higher risks of chronic disease.
- Women are more likely to experience autoimmune diseases.
- Men are at higher risk for cardiovascular conditions.
While we can’t change our biology, understanding genetic risk factors enables early screening and lifestyle modifications.
The Interplay of Determinants
Importantly, no determinant acts in isolation. They are deeply interconnected.
Example: A low-income family may live in a polluted neighborhood (environment), lack access to healthy food (behavior), have limited transportation (access), and experience high stress levels (social). Together, these factors compound to increase the risk of chronic illness.
Health inequities arise when people face systematic disadvantages in multiple determinants. Addressing these layers is key to promoting health equity.
Determinants in Action: Real-World Scenarios
1. The Urban vs. Rural Divide
In many countries, rural areas face shortages of healthcare providers, lower income opportunities, and fewer educational institutions. This results in higher rates of chronic disease and lower life expectancy.
2. Indigenous Communities
Indigenous populations worldwide often experience poorer health outcomes due to historical marginalization, economic exclusion, and cultural disconnection.
3. The COVID-19 Pandemic
The pandemic exposed the vulnerability of those with preexisting health conditions, low income, unstable jobs, and limited healthcare access. Social determinants shaped who was most affected.
Strategies to Address the Determinants of Health
To improve population health, interventions must go beyond clinical care to target root causes.
1. Policy and Legislation
Governments can implement policies to:
- Raise minimum wage
- Improve housing standards
- Regulate pollution
- Expand healthcare access
2. Community-Based Programs
Local initiatives that address food security, education, and mental health build resilience and improve outcomes.
3. Cross-Sector Collaboration
Health cannot be achieved by the health sector alone. Education, transportation, housing, agriculture, and justice sectors all play a role.
4. Empowerment and Equity
Engaging communities in decision-making ensures that solutions are culturally appropriate and sustainable. Health equity must be a guiding principle.
Technology and Determinants of Health
Digital health tools can bridge some gaps:
- Telemedicine improves access in remote areas.
- Mobile apps provide education and health tracking.
- AI-powered tools predict disease risk and target interventions.
However, digital solutions must be equitable. The digital divide—the gap between those with and without internet access—can worsen health disparities if not addressed.
Future Outlook: A Determinants-Focused Health Paradigm
As healthcare systems shift toward preventive care, addressing determinants is no longer optional—it is essential. The future of health depends on:
- Measuring social determinants in clinical practice.
- Training healthcare providers to understand social contexts.
- Embedding health equity in all policies.
- Involving communities in creating healthier environments.
Conclusion:
Health is shaped in our homes, schools, jobs, and communities. Medical care treats illness, but the determinants of health determine who gets sick in the first place.
Understanding and acting on these determinants allows us to build healthier societies, not just by treating disease, but by creating conditions where everyone has the opportunity to thrive.